Alzheimer’s diagnosis revamp embraces rating scale similar to cancer
2023.07.16 11:16
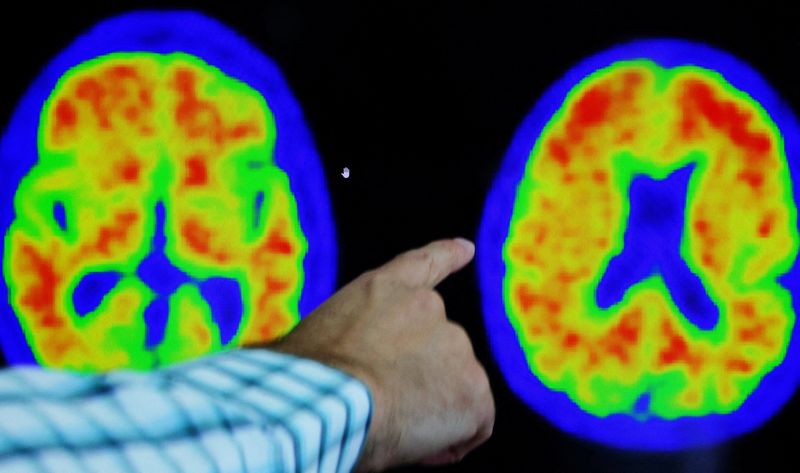
© Reuters. FILE PHOTO: Dr. Seth Gale points out evidence of Alzheimer?s disease on PET scans at the Center for Alzheimer Research and Treatment (CART) at Brigham And Women?s Hospital in Boston, Massachusetts, U.S., March 30, 2023. REUTERS/Brian Snyder/File Photo
By Julie Steenhuysen
(Reuters) – Alzheimer’s disease experts are revamping the way doctors diagnose patients with the progressive brain disorder – the most common type of dementia – adopting a seven-point rating scale based on cognitive and biological changes in the patient.
The new guidelines, unveiled by experts on Sunday in a report issued at an Alzheimer’s Association conference in Amsterdam, embrace a numerical staging system assessing disease progression similar to the one used in cancer diagnoses. They also eliminate the use of terms like mild, moderate and severe.
The revamp – replacing guidelines issued in 2018 – was prompted by the increased availability of tests detecting key Alzheimer’s-related proteins such as beta amyloid in the blood and new treatments that require confirmation of disease pathology prior to use.
The new system is designed to be more accurate and better reflect a person’s underlying disease, according to Dr. Clifford Jack of the Mayo Clinic in Rochester, Minnesota, lead author of the report sponsored by the Alzheimer’s Association and the National Institute of Aging, a part of the U.S. government’s National Institutes of Health.
The change comes at a time when doctors are preparing to identify and treat patients with Eisai and Biogen (NASDAQ:)’s drug Leqembi, which won Food and Drug Administration approval this month, and Eli Lilly (NYSE:)’s experimental drug donanemab, which is now under FDA review.
“We really are getting into an era of much more personalized medicine, where we’re starting to understand that there are certain biomarkers that are elevated to certain degrees in people in different stages,” said Dr. Maria Carrillo, chief scientific officer for the Alzheimer’s Association.
Under the new diagnostic approach, patients would receive a score of 1 to 7 based on the presence of abnormal disease biomarkers and the extent of cognitive changes. The system also includes four biological stages ranked a, b, c and d. For example, Stage 1a is when a person is completely asymptomatic but has abnormal biomarkers.
“Stage 1a is really the beginning of evidence that someone has the disease,” Jack said.
In Stage 2, an individual may have abnormal biomarkers and very subtle changes in cognition or behavior. Stage 3 is roughly equivalent to the current presymptomatic stage known as mild cognitive impairment, while stages 4, 5, and 6 are equivalent to mild, moderate and severe dementia.
The new scale also includes a Stage 0 for people who carry genes that guarantee they will develop Alzheimer’s. This category includes people with Down Syndrome, 75% of whom develop Alzheimer’s as adults.
Noting the new system’s similarity to cancer stages, Jack said, “There’s no such thing as mild breast cancer. They’re numeric stages.” Jack also noted that many other conditions can cause dementia but not all dementia is Alzheimer’s disease.
The new guidelines are intended for doctors to use in clinical practice as many face the prospect for the first time of offering patients treatments that can slow the course of the disease, rather than just treat symptoms.
Alzheimer’s, which gradually destroys memory and thinking skills, is characterized by changes in the brain including amyloid beta plaques and neurofibrillary, or tau, tangles that result in loss of neurons and their connections.
The 2018 guidelines, which were intended for research use, incorporated existing technologies for detecting Alzheimer’s proteins based on PET scans of the brain and tests of cerebrospinal fluid, which were only accessible via a lumbar puncture. Such tests were costly and not typically used in standard medical practice.








